Ontario Animal Health Network (OAHN) Bovine Expert Network Quarterly Veterinary Report
Look Out for Lead!
In 2023 there have been 3 cattle herds with lead toxicity in Ontario. Lead is one of the most common toxins in cattle. Cattle are curious and often indiscriminate feeders which puts them at risk when they encounter novel, discarded materials. Cattle are attracted to the metal taste and will actively seek it out.
Although lead cases are typically sporadic, they tend to happen when cattle are turned out to pastures that contain a lead source.
Signs of Lead Toxicity
- Die suddenly or are found down
- Depressed
- Appear blind
- Aimlessly wander, often separate from the herd
- Less commonly vocalize and be excitable
Although cattle of any age are at risk, young milk-fed calves absorb lead more effectively from their gastrointestinal tract, leading to greater susceptibility to lead toxicosis.
Prevention
- Prior to turning out cattle to new pasture, check for discarded materials since the area was last occupied by livestock
- Dispose of used batteries, paint, and oil properly at local collection stations for hazardous waste
- If a battery breaks open, the soil around the battery will be contaminated and should be cleaned up
Control
- To protect other cattle from possible lead poisoning, it is critical to identify the lead source and remove access.
- Some cattle can have elevated lead levels without showing outward signs of disease, however their meat and milk contain lead levels unsafe for human consumption. For this reason, all cattle exposed to the source of lead must be identified and tested.
Potential Sources of Lead
- Discarded batteries – Improperly discarded lead acid batteries from automobiles and farm machinery. Batteries that have been exposed to freeze-thaw cycles with damaged cases are easily accessed by cattle.
- Lead-based paints – Newer paints are virtually lead-free but older painted surfaces remain a risk. Cattle may lick old outbuildings or other painted surfaces or consume flaked paint chips. Lead also remains in the ashes from buildings that have burned.
- Discarded engine oil – Although unleaded gas has reduced the risk, old oil spills or dumpsites may still be contaminated.
- Farm machinery – May contain batteries, grease, used oil or filters containing lead.
- Roofing materials, plumbing supplies, lead shot and other waste can contain lead.
OAHN Trace Mineral Project Webinar Recording
In May, a webinar was held for veterinarians sharing a project summary and a presentation from trace mineral expert Dr. Cheryl Waldner on optimizing outcomes in cow-calf herds through more effective management of micronutrient supplementation programs.
To review the webinar, sign in via OAHN login and visit https://www.oahn.ca/resources/video-trace-status-in-ontario-beef-herds/
Trace Mineral Project Summary
Background
Trace minerals play an important role in cattle health, growth, immune function, and productivity. Supply of trace minerals to beef cattle can vary with soil type, pasture, forages and feedstuffs, supplementation formulations, and dry matter intake; and requirements vary with cattle age and production stage. Poor reproductive performance, reduced calf immunity, elevated calf morbidity, and reduced weight gain have been associated with trace mineral deficiency in cattle. Selenium deficient soils in Ontario, elevated molybdenum, and manganese deficiency associated with calves born shortened in stature have all been reported to the bovine Ontario Animal Health Network as concerns from veterinarians.
It is often impossible to directly measure trace mineral status in diets due to difficulties determining the dietary composition and the amount consumed, such as with pasture feeding. Blood samples can be utilized to directly measure the trace mineral status of cattle and is more practical.
Objectives
The objectives of the project were to:
- To determine mineral status of a selection of cows within beef herds across the province and assess risk for trace mineral disorders
- To provide veterinarians with the opportunity to assess mineral status in individual beef herds of interest and return findings to their producer to mitigate risk for trace mineral disorders
- To better understand mineral supplementation strategies employed by beef producers
Part 1 – Blood Sampling and Results
From October to December 2021, any Ontario veterinarian could enroll a herd in the project by submitting blood samples from 10 random mature beef cows to the Animal Health Lab (AHL).
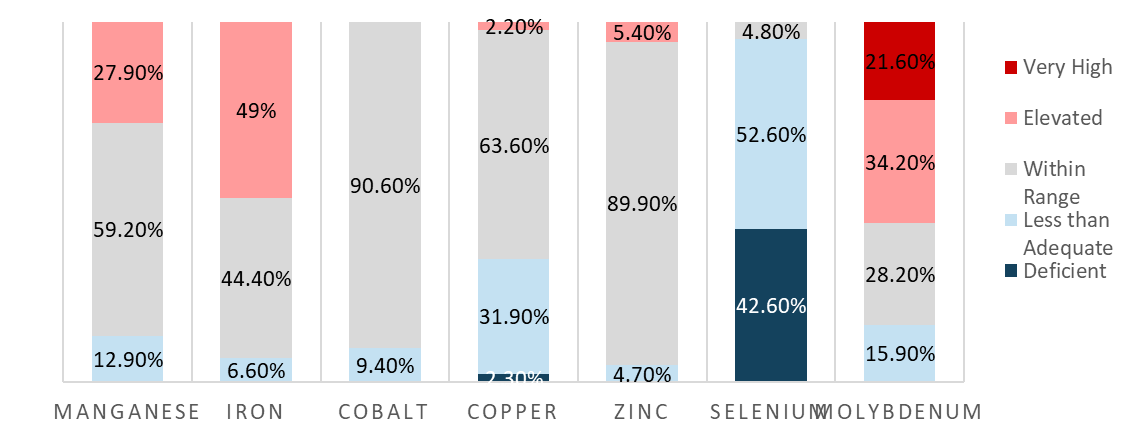
A project submission form collected information on the general herd characteristics, current supplementation strategies, and recent pregnancy diagnosis outcomes. All samples submitted were tested using the AHL trace mineral panel which included manganese, iron, cobalt, copper, zinc, selenium, and molybdenum. Results were returned to the veterinarian for use by the herd.
A total of 69 herds were enrolled in the project. The average number of cows was 44 (range 11-475) and the average number of heifers in the cow-calf herd was 10 (range 0-160). Herds were spread out across the province and included 15 in Southern Ontario, 23 in Western Ontario, 7 in Central Ontario, 17 in Eastern Ontario, and 7 in Northern Ontario.
All herds reported providing some form of mineral supplementation prebreeding, 95.6% of producers fed mineral at breeding and postbreeding, and 94.2% through gestation and precalving. Most producers reported using free choice mineral provision (n=59), and to a lesser extent mixed in a total mixed ration (n=10), mineral blocks (n=11), lick tubs (n=8), and injectable (n=2). Pregnancy success reported in cows averaged 94.4% and in heifers 91.7%.
The distribution of blood results is provided in Figure 1. The most significant abnormalities noted included 53% of samples for selenium being less than adequate (<0.08 ug/mL) and 43% deficient (<0.04 ug/mL), 49% of samples with elevated iron (>1.0 ug/mL), 32% of samples less than adequate for copper (<0.06 ug/mL) and 2.3% deficient for copper (≤0.03ug/mL), and 32% of samples elevated for molybdenum (<30ng/mL) and 22% of samples very high (>100ng/mL).
Many herds experienced several mineral abnormalities and mineral abnormalities tended to cluster in herds. Frequently all cows tested within a herd were low for selenium or high molybdenum. Because all herds were supplementing at one stage and the majority were supplementing at all stages, comments on the effects of supplementation on mineral status cannot be made.
Part 2 Survey of Management Practices
In December 2022, a follow up survey was sent to the producers that had participated in the project.
Results of the calving season reported 49% had experienced one or more stillborn calves (range 1-17% of calves), 60% had at least one weak born calf (range 1-6%), and 31% had at least one or more mortalities before 30 days of age (range 1-15% of calves). Only 2 herds indicated they had calves born with skeletal abnormalities or a shrunken stature (total or 3 calves in 2 herds). Other management practices described included 78% of herds vaccinated dams for neonatal diarrhea pathogens, 78% of herds giving selenium injections at birth to calves, and 61% of herds providing supplementary colostrum to a portion of calves as needed.
Using a retrospective approach to verify mineral fed, producers reported the amount of mineral fed/month, the weight per bag, the number of cows fed, and a mineral analysis from the product. Fifteen herds provided sufficient data to calculate the trace mineral supplementation rates in their herd. The mineral feeding rate ranged from 21 to 164 grams/head/day with a median of 75 grams/head/day. Three out of 15 herds fed sufficient selenium for a late gestation pregnant, average sized beef cow. Assuming a quarter of requirements are supplied by forage in the diet, projections for other minerals including copper, manganese, and zinc indicated 7, 3, and 5 herds supplied sufficient Cu, Mn, and Zn, respectively.
Discussion and Summary
Herds in the present study were more likely to offer mineral supplementation than in previous studies. Enrollment through the herd’s veterinarian means that herds were likely biased towards working with a veterinarian and other advisors, were willing to share their information knowing that a mineral feeding strategy was in place already and had an interest to monitor the farm’s current supplementation practices. Free choice supplement was a popular strategy among the herds enrolled. Many animals had abnormal trace mineral values, however the clinical significance of this is unknown. The most common abnormalities were high iron, low copper, low selenium and high molybdenum. Trace mineral abnormalities tended to cluster in herds and in individual animals. Pregnancy outcomes met targets for most herds enrolled and a small number of herds that completed the follow up survey reported deformed calves, stillbirths, weak born calves, or neonatal mortality. Where mineral delivery and product information was provided, many herds were under-delivering mineral.
Analysis of blood serum for trace mineral status is useful when liver samples cannot be accessed. A knowledge of individual serum reference ranges including the effects of physiologic state such as pregnancy and lactation is necessary to interpret results accurately. Most serum values reflect recent mineral supplementation, but there are exceptions such as copper. Taking samples from a proportion of the herd, in most cases at least 10 animals, reduces effects of random variation and gives an accurate herd picture.
The OAHN Bovine network has recently received approval for a new project testing a sample of blood samples from healthy dairy cattle to explore the presence of M.wenyonii and C.M haemobos in Ontario cattle populations and to produce KKT information for bovine veterinarians on the presentation and risk for M.wenyonii and C.M haemobos. Stay tuned!
Case Report: Mycoplasma wenyonii in dairy cattle
Dr. Kristen Edwards
A four-year old Holstein cow on a 200-cow closed dairy herd presented on April 29, 2017, with anorexia, anemia, and mild dehydration. She calved one day prior to initial presentation and was the third animal to display similar clinical signs. She had been previously housed outside as a dry cow along with other far-off cows. The first two cows displaying similar clinical signs were sent direct to slaughter with no intervention due to extremely low milk production and thus minimal financial incentive to treat. The decision was made to further investigate and determine a diagnosis when the third case was observed, as there was a concern that the problem was no longer at the individual animal level and instead could be herdwide with the risk of more animals becoming diseased. Physical examination revealed pallor and jaundice, normothermia (38.7°C), rumen stasis, tachycardia (92 beats per minute), and mild tachypnea (32 breaths per minute) with accompanying dyspnea. There was no evidence of external bleeding, internal bleeding such as uterine, or petechiae. Differential diagnoses included severe acute leptospirosis and anaplasmosis.
Blood was collected and sent for comprehensive complete blood count (CBC), biochemistry, blood smear cytology, and Anaplasma marginale competitive enzyme-linked immunosorbent assay (cELISA) testing. An additional Leptospira microscopic agglutination test (MAT) and haemoplasma PCR and sequencing test were requested. A provisional diagnosis of anaplasmosis was made and she was prescribed once daily 6.6 mg/kg intramuscular oxytetracycline hydrochloride for five days and daily 1 mL/45 kg intramuscular vitamin and amino acid injectable solution for the same duration.
Biochemistry revealed multiple abnormalities including hypocalcemia, hypophosphatemia, hyperhaptoglobinemia, and hyperbilirubinemia. CBC demonstrated an increase in white blood cells and mean corpuscular volume and a decrease in red blood cell count, hemoglobin, and hematocrit. Ghost cells and basophilic stippling were observed on manual differential, but no infectious agents were seen. No Anaplasma marginale organisms were visually identified on blood smear cytology. The cow was subsequently euthanized. She was in good body condition (3/5 body condition score) with markedly icteric udder, perineum, and mucous membranes. Grossly normal milk was expressed from all mammary quarters. Internally the carcass was diffusely pale, particularly the liver and heart, with watery blood throughout. The internal adipose reserves were markedly icteric and the omentum contained focal hemorrhages up to 10 cm in diameter. The interlobular septa of the lungs were diffusely expanded up to 1 cm with edema, most prominently in the dorsal lobes and suspected to be secondary to hypoproteinemia.
Grossly the necropsy could not identify the cause of the cow’s clinical signs but could not exclude hematogenous parasites and leptospirosis. The cELISA returned a negative result for Anaplasma marginale with a 17.78% inhibition. Additionally, leptospirosis testing for Leptospira species autumnalis, bratislava, canicola, grippotyphosa, hardjo, icterohaemorrhagiae, and pomona were all negative. An additional gel-based PCR for haemoplasmas was performed on May 11, 2017, and returned positive for Mycoplasma. On May 31, 2017, the results of the sequencing returned with a 99% similarity (498/499 bp) to Mycoplasma wenyonii.
Nine randomly selected, clinically healthy, pre-parturient cows were surveilled for infection on July 10, 2017, and blood was collected and sent for haemoplasma PCR and sequencing. Four of nine animals selected were positive for Mycoplasma wenyonii.
Global Surveillance Report
Salmonella I:4,5,12:i:− From RAIZO (Quebec)
From 2020 to 2022, an outbreak of 17 human cases caused by a multidrug-resistant strain of Salmonella I:4,5,12:i:− has been identified in Quebec. The majority of these cases involved children aged two years or younger. This same strain was identified during the same period in 11 calves and 1 moose that was in contact with cattle. For 14 of the 17 human cases, an investigation was carried out by public health authorities in collaboration with MAPAQ. For 8 of these 14 cases, or 57% of cases, direct contact with a dog that had a raw meat diet was confirmed. For the six other cases investigated, direct or indirect contact with cattle or consumption of beef were reported. Among others, an employee of a beef farm and the child of a beef calf breeder are part of these six cases. Zoonotic risk management is a challenge in raising calves struggling with this multi-resistant bacterium. The situation also highlights the public health risks associated with raw meat diets for pets.
Bovine Tuberculosis – From CFIA
A heifer that tested positive for bovine tuberculosis at a US slaughter plant was traced back to a domestic cattle herd in Saskatchewan. Subsequent testing results reported July 12-2023 found 8 additional positive animals in the herd of origin, now depopulated. Further trace-out and trace-in activities from this herd will take place over the next several months. CFIA reports at this time these new findings should not affect Canada’s current international status in which all provinces are considered bovine TB-free. Updates on the investigation are available at: Status of the bovine tuberculosis investigation – Canadian Food Inspection Agency (canada.ca)
Q1 Bovine Animal Health Laboratory Data
During Q1 (February 1 to April 30, 2023), there were 209 bovine pathology submissions to the AHL.
CASE HIGHLIGHTS
- History: 3 young calves on farm with history of progressive dysphagia and dyspnea after drinking milk. No significant lesions on gross PM, except for mild pneumonia.
- Findings: Ulcerative omasitis and rumenitis, peritonitis, multifocal hepatic and renal necrosis, fibrinosuppurative bronchopneumonia
- Summary: Aspiration pneumonia and rumen drinking. Suggestion to check nipple size/flow from bottles, as colostrum/milk replacer could be flooding the throat and upper GI tract.
- History: 5-month-old Holstein calf presented with acute collapse and inability to stay sternal, treated with antibiotics, dexamethasone, and thiamine for 3 days, and subsequently died.
- Findings: Subacute fibrinous and suppurative meningitis (brainstem/pituitary); Epicardial, interstitial and endocardial hemorrhage with multifocal fibrinoid necrosis/vasculitis.
- Summary: This calf had severe fibrinosuppurative meningitis, and PCR testing of the affected brainstem detected Mycoplasma bovis, consistent with a causal role in the development of this meningitis. There may have been concurrent bacterial infection, but bacterial culture of the meningeal swab and pooled tissues did not produce any bacterial growth, though these results may have been influenced by antimicrobial therapy. With the brain lesion serving as a nidus of infection, the gross and microscopic lesions in the heart are thought to be the result of a terminal systemic inflammatory response/septicemia.
- History: 1st lactation cow, 66 days in milk, aggressively licking her teats/udder around the time of calving and has been since. The behavior resulted in significant trauma to her teats (most severely RF and LH). This problem had been noted in approximately one fresh heifer every 12-18 months. It is challenging to manage and use of a bra, attempts to alter her behavioural time budget and access to her udder were ultimately not successful in preventing this cow from causing further damage to her teats/udder.
- Findings: Chronic mastitis with necrosis, fibrosis, and self-mutilation of teats
- Summary: Cause for teat self-mutilation not determined
- History Case A: 2-year-old Angus, outbreak of pneumonia; Vaccine status not up-to-date.
- History Case B: 3-year-old Angus died acutely, no clinical signs prior.
- Findings: In both cases, the animals had necrotizing eosinophilic bronchointerstitial pneumonia with microscopic identification of larvae within the pulmonary lesion in case A, and eosinophilic enterocolitis with nematode larva identified in case B. Case A also had mild hepatitis and focal eosinophilic lymphadenitis.
- Summary: These were two cases of verminous pneumonia. Based on the morphology of the parasite in histologic sections and the history of pigs in the barns, Ascaris suum is most likely. Ascaris suum eggs are extremely hardy and long lived in the environment. There is a bovine roundworm (Toxocara viturolum), but it is uncommon in North America, and infection is largely asymptomatic in adult cattle.
SALMONELLA
In total, 229 bovine submissions had bacterial culture performed (non-milk), generating 340 cultures. Salmonella spp. were isolated from 27 submissions, representing an estimated 16 premises.
- Salmonella Dublin was isolated from 6 submissions, representing approximately 5 premises. Primary findings associated with isolation of S. Dublin (if provided), included pneumonia, diarrhea, and sepsis.
- Salmonella Typhimurium and Salmonella Agona were isolated from enrichment in two separate cases of diarrhea in 1- to 2-week-old calves that had PCR detection of rotavirus and coronavirus (no pathology performed)
BOVINE VIRAL DIARRHEA VIRUS (BVDV)
In total, 56 submissions generated 282 BVDV PCR tests, one BVDV type 1 positive result
- 5-month-old Holstein calf, reported to be BVDV-immunoperoxidase positive and antibody negative (compatible with a PI)
In total, 2 pathology submissions had BVDV immunohistochemistry performed, both of which were negative.
- 1-week-old lamb born ataxic in the hind end
- Ear notches to assess for PI animal (IHC is no longer routinely performed for PI screening). See the AHL website for more information regarding current recommendations for BVDV testing: https://www.uoguelph.ca/ahl/labnote-1-summary-bovine-viral-diarrhea-virus-bvdv-testing-ahl
Latest Podcast: Johne’s Disease Control on Ontario Dairy Farms
Dr. Jamie Imada joins the OAHN bovine network to discuss his thesis, “A Holistic Investigation of Johne’s Disease Control on Ontario Dairy Farms through Quantitative and Qualitative Methods”. Dr. Imada discusses the results of follow up risk assessment and management plans (RAMPs) on 180 Ontario dairy farms and the changes in management practices on study farms since the end of the Ontario Johne’s Education and Management Assistance Program in 2013, the current prevalence of Johne’s Disease (JD) in Ontario, and the motivations and barriers for producers with regards to JD control and farm biosecurity.
Check is out at http://oahn.podbean.com
Help us help you!
Have an idea for an infographic you’d like to see, or a podcast you’d like to hear? Email oahn@uoguelph.ca to let us know!